Active Monitoring - A Day In The Life of a Practitioner

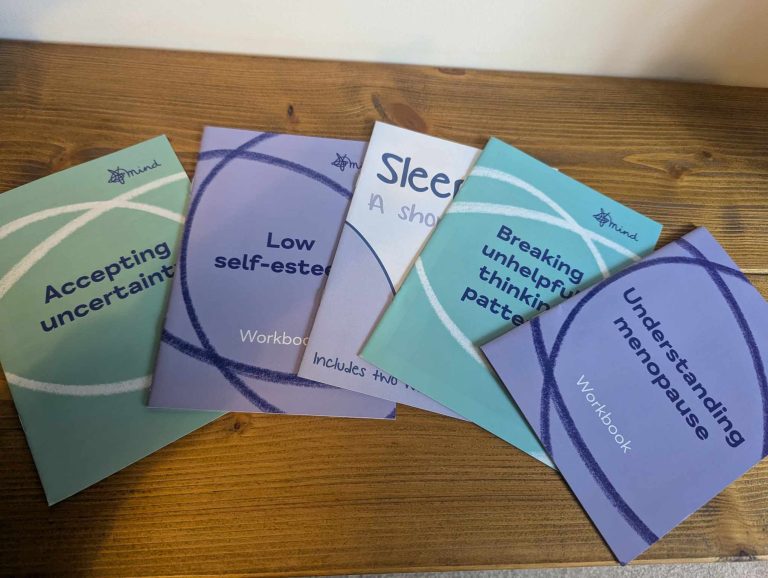
Active Monitoring (AM) is a guided self-help support service for low to moderate mental health difficulties, such as anxiety, low mood, anger, stress, low self-esteem, loneliness, grief and loss and understanding menopause. The service is a patient-centred, early intervention, consisting of 5 face-to-face sessions, based within GP practices across South Warwickshire, Evesham, Bredon, Broadway and Inkberrow. Below is an example of a typical day for an AM Practitioner.
8:30am – 9:00am: Arrive at surgery, ensure room is appropriately equipped, log into clinical systems. Plan day ahead – ensure prepped with patient notes, gather resource for sessions, print wellbeing measures.
9:00am – 9:30am: Session 1 – Continuing loneliness support. Reflect upon previous session and discuss improvements in patients’ wellbeing. Discuss information researched for patient regarding local social groups and exercise classes. Discuss SMART goals and how this may improve confidence. Contact GP upon patient’s request regarding physical health concern.
9:30am – 10:30am: Information Gathering Appointment – New referral Introduce service, explain confidentiality and complete wellbeing measures. Give patient time and space to discuss their feelings of stress and anxiety and their expectations for support. Give empathetic listening and reassurance. Provide psychoeducation and resources regarding anxiety and stress. Discuss benefits of breathing techniques, exercise and self-care for managing anxiety and stress. Discuss the relationship between thoughts and feelings, unhelpful thinking patterns for mood and ways we can challenge these.

10:30am– 11:00am: Admin – Respond to emails and research additional support services for patients.
11:00am – 11:30am: Session 5 – Ending low mood and anxiety support. Take wellbeing measures; give encouragement towards patients significant decrease in anxiety and depression and significant improvement in wellbeing. Reflect upon coping strategies they have adopted and give encouragement to continue these. Discuss and provide signposting options for future support, should patient require.
11:30am – 12:00pm: Additional Session – Ending support for anger management and depression. Discuss signposting options for further support – local courses for anger management, as well as peer support and social groups, mood-masters courses and other apps and professional services available for depression.

12:00pm – 12:30pm: AM Session 3 – Continuing anxiety support. Reflect upon previous session, answer any questions regarding resources. Discuss improvements in patients’ wellbeing and reflect upon coping strategies they had adopted from mindfulness and accepting uncertainty resources. Take wellbeing measures taken as a mid-support check; give encouragement regarding patient’s anxiety significantly decreasing, and wellbeing significantly increasing since initial appointment. Encourage them to continue utilising coping strategies. Discuss how accepting anxiety using POWER and considering alternate perspectives can help further with managing anxiety.
12:30pm – 1:00pm: Admin – message GPs and other staff any concerns/ enquiries patient has requested and update clinical systems with morning session notes.
1:00pm – 1:30pm: Lunch break – Wellbeing Walk, eat lunch.

1:30pm – 2:00pm: Session 2 – Continuing low self-esteem support. Give time and space for the patient to discuss their self-esteem and lack of confidence. Reflect upon discussion and discuss how recording an achievement, closeness and enjoyment log may help them to identify activities which boost or impact their self-esteem. Discuss how negative thoughts about self can influence feelings towards self, and ways in which we can challenge these thoughts. Discuss writing a compassionate letter to self.
2:00pm – 2:30pm: AM Session 4 – Coping with grief and loss support. Discuss improvements in patients’ wellbeing and reflect upon coping strategies they find beneficial. Discuss personal support kit as a reminder for coping strategies. Give time and space for patient to discuss recent concerns; give empathetic listening. Discuss keeping a gratitude diary and benefits of focusing on positives for mood.
2:30pm – 3:30pm: Information Gathering Appointment – New referral Introduce service, explain confidentiality and complete wellbeing measures. Give time and space for patient to discuss their struggles with
low mood and sleep and their expectations for support. Give empathetic listening and reassurance. Discuss sleep hygiene and the impact lack of sleep can have on mood. Discuss coping strategies for low mood and improving wellbeing. Discuss thoughts and feelings diary and how reflecting on situations where we felt low can help identify unhelpful thinking patterns or behaviours.
3:30pm – 4:00pm: Admin – message GPs and other staff any concerns/ enquiries patient has requested and update clinical systems with afternoon session notes.