The Impact of Suicide... A Personal Story

In 2008, our colleague Emily tragically lost her brother to suicide. In this blog, she recounts her upbringing with a sibling struggling with mental health issues, and explores how his behaviour ultimately contributed to him taking his life…
“People often ask me when it was that I first noticed my elder brother Ben had mental health problems and the answer is, I just don’t know.
That’s the thing about mental illness, it can very often be just that; this ‘thing’ that slowly creeps up on you over a period of months or even years, and then bam, suddenly you realise you’ve got these issues that may feel insurmountable.
Ben was 32 when he took his own life. Although it was nearly 15 years ago, I remember my dad coming through the front door in the small hours to tell me like it was yesterday. Despite the fact he’d suffered with poor mental health a lot in his life, nothing prepares you for the shock of that devastating news. It ripped a hole in our hearts.
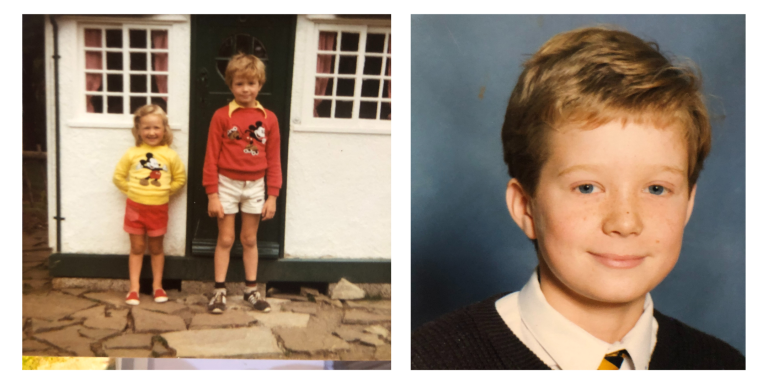
Rewind back to our childhood years (Ben was two and a half years older than me) and things weren’t often easy. From the outside, in the earlier period at least, our family probably looked like a typical one, one with a fair amount of sibling rivalry. But it felt like a whole lot more than that to me.
Ben got a paper round when he was 13, and he lacked any motivation to get up and out the house in the morning. I would hear frequent raised voices and frayed tempers when my parents were trying to get him out of bed. More often than not, my dad would go and do the paper round for him. On the flipside, I was the child that towed the line, tried hard at school, ticked all the ‘well behaved’ boxes. Looking back, I just think we were wired differently, although that’s not to say I didn’t go through my own rebellious phase. Likewise, it’s certainly not to say I was immune from mental health problems myself, I’ve had my own over the years.
This lack of motivation that Ben displayed was possibly the start of his decline. It manifested itself in different ways, and it meant that he was easily led and influenced, he went along with the crowd. Sadly, his ‘crowd’ wanted to try cigarettes and alcohol at 13 and start skipping school at 14. Later on, they would go on to experiment with drugs, display antisocial behaviour, sometimes getting into trouble with the police. The trouble was, I’m pretty sure Ben had an addictive personality, so whereas some people would have the ability to draw a line, ‘grow up’ and turn their back on that lifestyle, Ben just didn’t seem to have this capability.

In addition to this, I believe he also suffered from generalised anxiety disorder. During his secondary school years and right through to adulthood, he worried (irrationally, in my opinion) about the shape of his head and also the fact that he had a slightly concave chest. Though these would be barely noticeable to anyone else, he would spend hours looking at his reflection in the mirror, and talk for hours into the night with mum about it.
Despite this, Ben had many positive attributes. He could be very caring, he loved his family unit, and he was often protective of his closest relatives. He adored our extended family holidays camping in France and going out to eat with mum, dad and me. Academically, his school reports would often mention the huge potential Ben had, but sadly this was never realised.

Ben left school after his GCSEs (none of which he passed) and from there, his mental health went on a downward trajectory, interspersed with the odd ray of hope. He got an apprentice YTS role with IBM, but they let him go shortly after he started because he just didn’t show up half the time. He got a string of other jobs following this, but they ended the same way. He had an off-on problem with alcohol and drugs, which contributed to a whole host of other issues like aggression, depression, paranoia and anxiety. Later on, when he described episodes where he could hear voices come through to him from the telly, it was suggested by the GP that he might be suffering from borderline schizophrenia.
It was around this time that he was referred to St Michael’s Psychiatric Hospital for support, which became a regular feature of his life. He was often admitted as an inpatient, and on one occasion stayed for a year. He was on constant medication. By this point he had moved out of our parents’ home, starting off in his own flat nearby. Later on, he would move into a house share in Leamington, living with other people with mental health problems.
He started on a vicious circle of taking medication, then taking himself off it because he felt better. This of course led to his condition deteriorating, which caused more self-destructive behaviour, whether that be more drinking, spending long periods on his own gaming, or watching TV all night, and eating extremely poorly, which in turn led to aggression, fatigue or extreme depression. On one occasion, he accidentally cut himself whilst separating frozen burgers and nearly bled to death, and on two other occasions, he tried to overdose. He nearly caused a fire when he fell asleep with a cigarette in his hand, that happened on multiple occasions.
One time in 2003, when I was living 100 miles away in South London in a house share with friends, he somehow travelled all the way down from Warwickshire in the middle of the night, under the influence of something. He found our house and knocked furiously on the door at 4am, frightening the life out of my housemates. To this day, in what was a pre-social media and smart phone era, I’ve no idea how he found me. I’d never given him my address and as an impulsive person, I’d be surprised if he’d done any research ahead of that to find out where I was. He was barefoot, his feet were wrinkled and white, like they’d been in water for hours. He was shivering, pretty confused and extremely agitated.
In order to stop him controlling his own medication, doctors administered them by depot injection, which brought with it a whole host of different side-effects including weight gain and extreme lethargy. He had to turn in his driving licence which severely impacted his independence and emotional wellbeing.

Fast forward five years, by this time I’ve got two young kids, aged three and 18 months. Ben and I went round Stratford Mop (a street fair) with them. It was a lovely evening, Ben was great with the kids, he bought Grace a candy necklace and took Isaac on a couple of baby rides. I had a bit of a moan at him for going on some of the big rides by himself, saying he could go another time, I’m so cross with myself for saying that now. But all in all, he was in fairly good spirits, I thought his mood seemed very stable. At the end of the evening, we said our farewells and went our separate ways.
That was the last time I saw him. Two days later, he took his own life, he’d jumped in front of a coach on a busy road in Leamington. I talked earlier about Ben being impulsive, and I feel like this was exactly that. He’d left no note, and offered no warning, he’d even left his phone on charge.
At his inquest, the coroner agreed with this, and said if the circumstances hadn’t presented themselves the way they did on that night, he may well have headed home and put the kettle on. I went to a group clairvoyant evening a few days later (my mum had already bought a ticket before he died and asked me to go), and Ben came through, saying he’d simply ‘had enough.’
I’m not really sure how I feel about all of this, but I do know it throws up so many unanswered questions. What made him do what he did, what flicked the switch? Why didn’t he reach out or give us any indication? Should I have picked up on any signs? If he’d been formally diagnosed, would he have managed to make a recovery? Ultimately, was his suicide preventable, or would he have tried again?
Looking back now, with so much more information now at our disposal, I find it strange more wasn’t done to offer him a formal diagnosis. I often wonder whether he was bipolar, had another type of personality disorder, or even whether he had a developmental disorder such as autism.
In addition to the questions, I know I have huge feelings of guilt. Guilt that I was a bit grumpy on the night of the fair. Guilty I couldn’t do more to save him. Tragically, our dad passed away to cancer just five months later; and I feel guilty that I feel angry at Ben for leaving me to pick up the pieces of what was left of our shattered family.
A decade and a half later, now finding myself working for a local mental health charity, I can certainly reflect on his death with more perspective. Maybe Ben couldn’t be saved, we’ll never know. But, as a society, as a community, we have to assume that everyone can be saved, that is our duty, and we should never stop trying.
Charities like South Warwickshire & Worcestershire Mind continue to reduce the stigma attached to mental health and help sufferers access support. All the sorts of stuff that Ben would’ve benefited from, were he here today.”
If you’re suffering from mental ill-health, or you know someone who is, you can contact these numbers in an emergency. Alternatively, these are the services that SWWMind offer across the region:
Supported Self Help (Active Monitoring) – South Warwickshire
Supported Self Help (formerly Active Monitoring) is a program of five face-to-face sessions. As an early intervention program, it works in partnership with GPs to refer patients directly to an Supported Self Help Practitioner within the GP surgery as soon as they present with symptoms of anxiety and panic attacks, anger, depression, low self-esteem, stress, feeling alone and bereavement. Find out more here.
Worcestershire & Herefordshire Crisis Line
Our telephone line is available 24 hours a day, 365 days a year to Worcestershire & Herefordshire residents. We will determine the nature of your problem, the urgency of the situation and the most appropriate next step. Calls will be triaged and referred to the Crisis Resolution Team or guided to other appropriate support. Find out more here.
Worcestershire Safe Haven
This service runs seven days a week 18.00 – 01.00 and is based in the Redditch town centre. We provide telephone support and face-to-face appointments to Worcestershire and Herefordshire residents who are experiencing a mental health crisis. Find out more here.
Wellbeing for Warwickshire
Across Warwickshire, this service seeks to help Warwickshire residents through a 24 hour helpline, face to face support and wellbeing groups. Find out more here.
